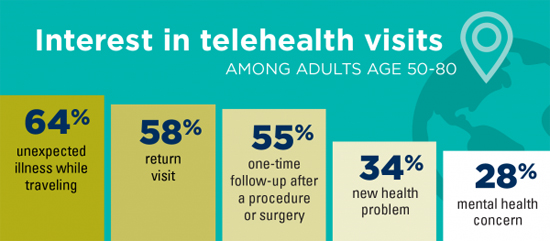
Virtual Medical Visits Get Wary Welcome From Older Adults, Poll FindsFew over 50 have tried telehealth and most see in-person care as better—but one-half would consider it for encounters with their primary providers. The technology is there. The funding is nearly there. The health providers are getting there. But a new national poll suggests that people over 50 aren’t quite ready to fully embrace virtual health visits with their doctors and other providers—also known as telehealth. Only 4% of those polled by the National Poll on Healthy Aging had had a video-based telehealth visit with a provider via smartphone or computer in the past year. Their reactions were mixed. Meanwhile, more than one-half of all those polled didn’t know if their health providers offer telehealth visits at all. More than 80% of older adults polled expressed at least one concern about seeing a doctor or other provider virtually rather than in person. And 47% worried about getting the technology to work. But more than one-half said they’d be willing to try telehealth in some situations, for instance if they got sick while traveling or needed follow-up on previous care. The poll, carried out by the University of Michigan (U-M) Institute for Healthcare Policy and Innovation with support from AARP and Michigan Medicine, U-M’s academic medical center, involved a national sample of more than 2,250 adults aged 50 to 80. They answered questions about many aspects of video-based telehealth. Among the one-third of poll respondents whose health providers don’t yet offer telehealth, 48% said they’d be interested in trying it with their primary care provider. But fewer would try it for specialty or mental health care.
Key findings from the telehealth poll conducted by the National Poll on Healthy Aging “As telehealth finally appears poised to live up to its potential, with insurance reimbursement in place or set to begin soon under many plans, and providers increasingly investing in systems, these poll data show a need to focus on the patient side,” says Jacob Kurlander, MD, MS, a U-M and VA Ann Arbor Healthcare System gastroenterology specialist and telehealth researcher who helped lead the poll. “As the industry moves forward, we should heed the concerns and preferences of our patients, especially those over age 50, who use the most health care.” Preeti Malani, MD, the poll’s director and a professor of internal medicine at U-M, notes that focusing on certain types of telehealth visits might be a way to help older adults get comfortable with the concept and see its value. “Telehealth won’t replace in-person medical examinations completely, but for situations where in-person visits aren’t essential, they can save time and resources for patients and providers alike,” she says. “Providers shouldn’t assume older adults aren’t receptive to virtual visits, but they should understand and work to overcome some of the reasons for hesitation.” For instance, she points to the 64% of respondents who said they’d be interested in telehealth options if they became unexpectedly ill while traveling, and the 58% who said they’d be interested in using it for a return visit after seeing a provider in person for an issue. But 71% were concerned that providers couldn’t do a physical exam over a webcam or smartphone camera, and 68% worried the quality of care they’d receive wouldn’t be as good. Indeed, among the small minority who had used telehealth, 58% said they felt that office visits offered better quality of care. Nearly one-half were concerned about privacy. Low Use, High Potential Some of those changes will specifically affect older adults. Starting in 2020, Medicare Advantage HMO insurance plans will be able to reimburse health care providers for seeing patients via computer or smartphone. Veterans have increasing access to telehealth, as do people who receive their health coverage through their employer or Medicaid. But providers that have begun to offer telehealth options may need to do a better job of letting their older patients know it’s an option, and helping them understand how it works, the poll suggests. “Many older Americans can benefit from being able to get care through telehealth without long trips to their doctor’s office,” says Alison Bryant, PhD, senior vice president of research for AARP. “Telehealth allows people to schedule health-related appointments, request prescription refills, and link to health care providers when time or distance is a barrier. It can also support family caregivers who are taking care of their loved ones.” What This Means for Providers and Payers “Especially for patient with mobility and transportation issues, who live in rural areas, or who live far from specialty care providers, telehealth could be an important improvement in access,” says Saini, a U-M gastroenterologist and VA Center for Clinical Management Research acting director who is studying the use of telehealth in specialty care. “But we will need evidence-based approaches to sustain and increase participation.” At CCMR, Saini directs the Program on Access, Community Care, and Specialty Care Services (ProACCeSS). The National Poll on Healthy Aging results are based on responses from a nationally representative sample of 2,256 adults aged 50 to 80 who answered a wide range of questions online. Questions were written, and data interpreted and compiled, by the IHPI team. Laptops and Internet access were provided to poll respondents who did not already have them. Source: Michigan Medicine - University of Michigan |